Providing access to psychosocial support for forcibly displaced persons: Q&A with Moses Mukasa
10 October 2023

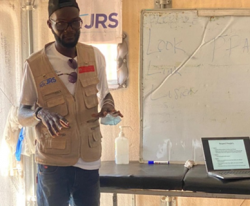 Moses Mukasa has been working for about a decade to promote access to Mental Health and Psychosocial Support (MHPSS) in humanitarian settings, particularly to populations affected by conflict and forced displacement, so that they can promote, rebuild, and sustain their resilience. Inspired by the words of Fr Pedro Arrupe SJ “to be with rather than to do for”, Moses joined JRS in April 2023 as an Inter-regional MHPSS Officer for the Eastern and Southern Africa regions.
Moses Mukasa has been working for about a decade to promote access to Mental Health and Psychosocial Support (MHPSS) in humanitarian settings, particularly to populations affected by conflict and forced displacement, so that they can promote, rebuild, and sustain their resilience. Inspired by the words of Fr Pedro Arrupe SJ “to be with rather than to do for”, Moses joined JRS in April 2023 as an Inter-regional MHPSS Officer for the Eastern and Southern Africa regions.
Why is it important to provide mental health services and psychosocial support to forcibly displaced persons?
Access to mental health and psychosocial support is important for everyone, everywhere in the world. All people, regardless of their personal background and geographical location, have the right to be protected from all possible mental health risks and to receive available, accessible, acceptable, and good-quality MHPSS care. This, in a humanitarian context, is even more necessary. Forced displacement can cause very deep psychological wounds dictated by human rights abuses, deprivation, significant losses, disruption of family ties and networks, and social identity, and the loss of livelihoods often undermines people’s ability to continue their lives. Without addressing mental health issues, communities cannot fully recover from memories of conflict and displacement, but more importantly, in refugee contexts, they cannot easily become productive members of host communities. Therefore, actions to address the impacts of forced displacement and provide support to affected populations are very important.
How is JRS ensuring the provision of MHPSS worldwide?
At the institutional level, mental health and psychosocial support is one of the four priorities of JRS. Our approach to MHPSS is based on the notion and experience that wellbeing is multidimensional and depends to a large extent on multi-sectoral interventions. For these reasons, we moved from implementing MHPSS as an independent humanitarian action to integrating it with all other JRS areas of intervention. Improving psychosocial wellbeing is crucial and fundamental to ensure poverty reduction, quality education, effective livelihoods, advocacy, reconciliation, and peacebuilding, addressing protection risks, and rebuilding a sense of hope for the future. What I have observed over time is the importance of implementing a continuum of interventions covering the different layers of the Inter-Agency Standing Committee (IASC) MHPSS pyramid from basic services to clinical care in a community-based approach. Facilitating access to multilayered MHPSS programmes built on the principle of universality, strength, and resilience among forcibly displaced persons stimulates recovery and is essential for both the immediate wellbeing of the individuals, community members as well as for the long-term peacebuilding and reconciliation with oneself and the past.
What are the main challenges people forced to flee face in accessing mental health and psychosocial support services?
Despite the documented facts about the mental health and psychosocial needs of people forced to flee, access to meaningful and quality mental health and psychosocial support services remains a challenge that we can attribute to several factors. Firstly, the fact that MHPSS is an area and activity considered less of a priority, due to the limited understanding of what it is and the difficulties in adopting a multi-sectoral approach. While, secondly, on the side of those we serve, barriers to accessing mental health support include difficulty in communicating distress, stigmatising beliefs, shame, a preference for self-sufficiency, and the expectation that help will be difficult to obtain.
How can we overcome them?
From a macro perspective, overcoming these challenges involves adopting a multi-sectoral approach to mental health and psychosocial support. This means integrating MHPSS into each of the areas of intervention, from education to livelihoods to advocacy and reconciliation. On the other hand, from a micro perspective, more should be done on MHPSS awareness-raising at all levels of action, from the people we serve, to aid workers, to the decision-making tables. This would allow a more effective understanding of mental health disorders and the actions needed to address them, reducing, or eliminating the stigma, isolation, and myths that accompany MHPSS services and needs. Most of the MHPSS interventions we see in humanitarian settings have been based on “ways of thinking” that originated in Western countries, including a medicalised and psychiatric approach to wellbeing. The risk of applying this view of psychosocial wellbeing is to impose a practice that does not fit with local beliefs and culture. Therefore, contextualisation and a de-medicalised vision of peoples’ psychosocial needs is key in addressing most of the MHPSS challenges, especially those with underlying social and protection causes.
A final point I want to emphasise concerns the responsiveness of the communities. As humanitarian actors, we should recognise the capacities we can leverage. All communities and individuals have resources and strategies to deal with hardship, illness, and distress. Mobilising community effectiveness and leveraging capacities and resources can help people heal organically. It is the responsibility of humanitarian workers to respect, understand, and enable the community and individuals to heal.
Could you tell us about a significant episode where you witnessed the impact of psychosocial support on the people we serve?
The conflict in Sudan has had a very heavy impact on the mental and psychosocial health of individuals, families, and communities, to the extent that we have sometimes observed that people’s ability to cope has been overburdened.
Our community based MHPSS intervention in Renk, South Sudan, is a clear example of how psychosocial support repairs lives even in contexts of extreme despair and despondency. The programme focuses on providing psychological first aid, psychoeducation, community capacity building, and physiotherapy to members with specific needs with the aim of restoring emotional, psychological, and social relief and wellbeing. Through this approach, we also aim to mobilise people to use their own resources and capacities for resilience and community rebuilding.
What does accompaniment mean to you?
Accompaniment means going along and hand in hand with those we serve, diminishing power structures and hierarchical interrelationships between the JRS team, the actions, and the people we serve. Guided by this principle, our MHPSS work is a process of working together, trusting, and accompanying communities, ensuring that we work as one body and spirit. Ensuring that we are walking and co-creating together with refugees, through listening, supporting, and building hope.


